Artificial womb advancing
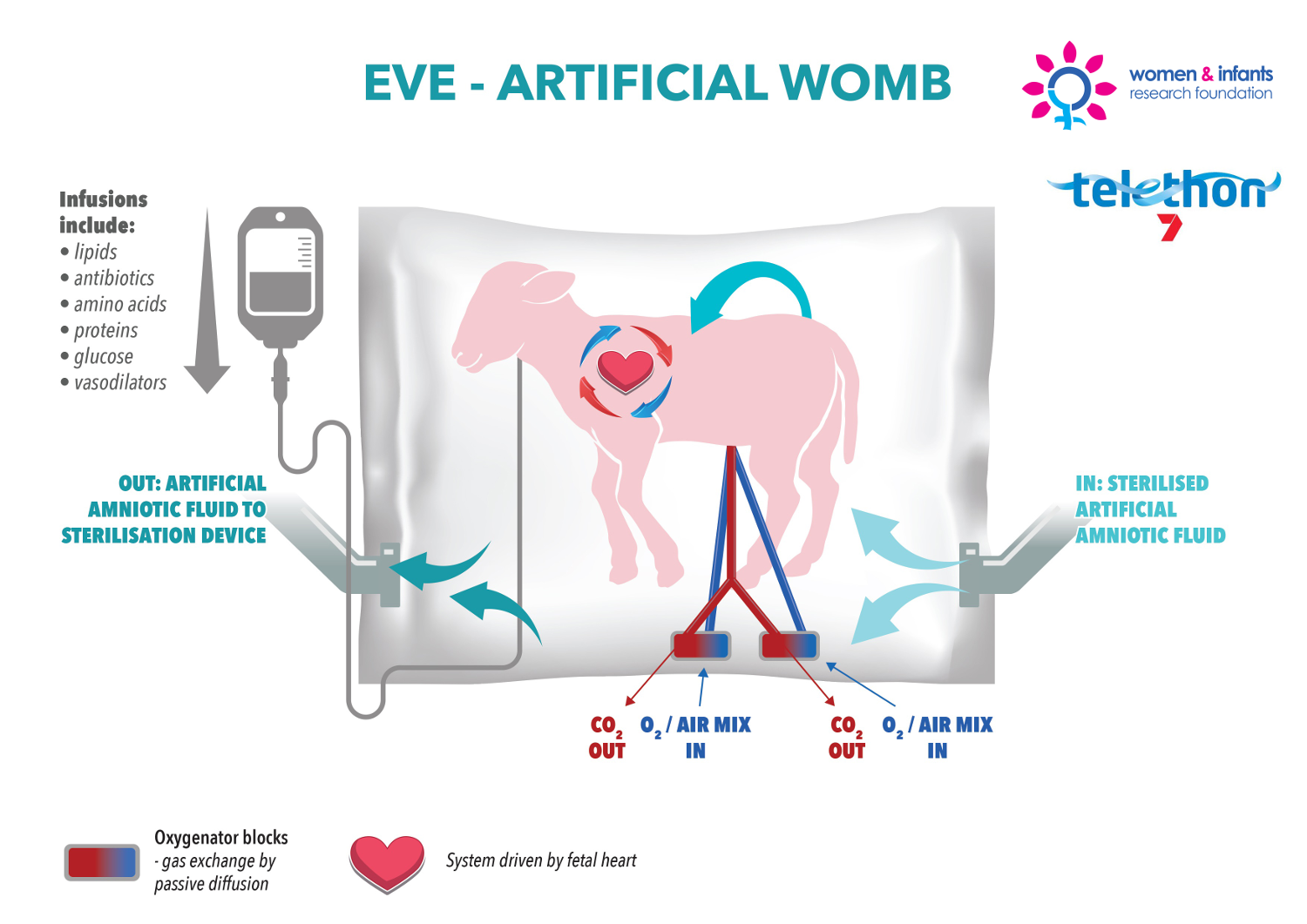 Australian researchers are working on an artificial womb – a placenta-filled bag that could one day save the lives of extremely premature babies.
Australian researchers are working on an artificial womb – a placenta-filled bag that could one day save the lives of extremely premature babies.
The artificial womb made headlines back in 2017 when it was first used to keep unborn lambs alive, but new studies have pushed back the date at which the device can be used.
A new study presents world-first data demonstrating the ability of an artificial placenta-based life support platform to maintain extremely preterm lamb foetuses (600-700g); equivalent to a human foetus at 24 weeks of gestation.
While previous research had demonstrated the feasibility of extended survival with artificial placenta technology in late preterm foetuses, there was no published evidence that demonstrated the use of the platform to support extremely preterm foetuses - the eventual clinical target of this technology.
“For several decades there has been little improvement in outcomes of extremely preterm infants born at the border of viability (21-24 weeks gestation),” says Associate Professor Matt Kemp from the Women and Infants Research Foundation.
“We have proven the use of this technology to support, for the first time, extremely preterm lambs equivalent to 24 weeks of human gestation in a stable, growth-normal state for five days.
“This result underscores the potential clinical application of this technology for extremely preterm infants born at the border of viability. In the world of artificial placenta technology, we have effectively broken the 4 minute mile.”
He says it is a significant milestone in the technology’s future implementation into clinical use.
“If we are to improve outcomes for babies born at the border of viability we must recognise that they are not ‘small babies’; rather, they are a unique patient demographic that, due to their extremely underdeveloped lungs and limited cardiovascular capacity, require an entirely different treatment approach from older preterm infants,” A/Prof Kemp said.
“The technology was designed to revolutionise the treatment of severely premature newborns. The goal is to offer a bridge between a natural womb and the outside world to give babies born at the earliest gestational ages more time for their fragile lungs to mature.
“With additional refinement, what today might be considered as futuristic technology might soon not be so futuristic and might be standard of care.”








 Print
Print