Cells set on tumour response
 Exposing cancers to bacteria can remind ‘first responder’ immune cells which side they are on.
Exposing cancers to bacteria can remind ‘first responder’ immune cells which side they are on.
According to new research, introducing bacteria to a tumour’s microenvironment creates a state of acute inflammation that triggers the immune system’s primary responder cells to attack rather than protect a tumour.
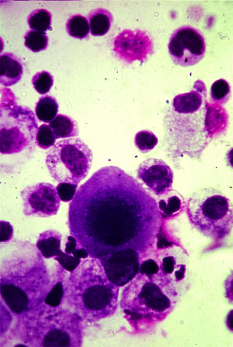
The ‘first-responder’ cells, called neutrophils, are white blood cells that play an important role in defence against infection.
While they generally protect against disease, they are notorious for promoting tumour growth; high levels of them in the blood are typically associated with poorer outcomes in cancer, in part because they produce molecules that shield the tumour by suppressing the other elements of the immune system.
Researchers, led by Dr Tatyana Chtanova, Head of the Innate and Tumour Immunology Lab at Garvan and Associate Professor at the School of Biotechnology and Biomolecular Sciences at UNSW Sydney, have found that injecting inactivated Staphylococcus aureus microbes inside a tumour reverses that protective activity, stimulating the neutrophils to destroy the tumour in a range of animal cancer models, including Lewis lung carcinoma, triple-negative breast cancer, melanoma and pancreatic cancer.
“Using the immune system to fight cancer has been one of the biggest breakthroughs in cancer therapy in the last two decades, but currently immunotherapy for improving T cell function doesn’t work for all types of cancer. We decided to use a different type of immunotherapy that targets neutrophils, to understand how generating acute inflammation in the immunosuppressive tumour microenvironment affects outcomes,” says Dr Chtanova.
The team used intravital imaging in animal studies to see inside the tumours in real time.
“Since attacking bacteria is the reason for neutrophils’ existence, we had a good inkling that introducing bacteria would bring neutrophils to the site and activate them. We discovered that it’s very effective in getting them to kill the tumours, chewing up their matrix,” she says.
The study, published in the journal Cancer Research, shows that the neutrophils also change at the gene expression level: they begin to secrete molecules that will attract fighter T cells as reinforcement.
“We’ve shown that microbial therapy is an effective booster for checkpoint inhibitor therapy, another type of cancer immunotherapy. We hope this synergistic effect will ultimately lead to better treatments to improve outcomes for patients with advanced or previously untreatable cancers,” says first author of the study, Dr Andrew Yam, clinical medical oncologist at The Kinghorn Cancer Centre and PhD student at Garvan.
The study focused on primary tumours. Over the next three to five years, the team will develop the therapy to fight metastasis, the spread of cancer to other areas of the body, with clinical trials to follow.








 Print
Print